Sexually active teenagers are generally responsible, but some don’t use contraception and a small percentage have sex that results in a pregnancy.
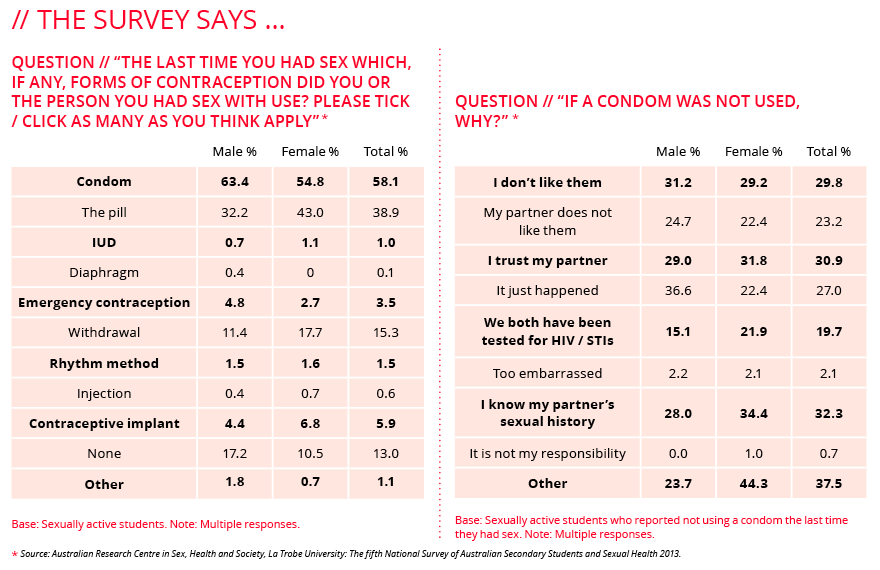
The fifth National Survey of Australian Secondary Students and Sexual Health 2013 (Australian Research Centre in Sex, Health and Society, La Trobe University) found 58 per cent of sexually active secondary students used a condom and 39 per cent used the contraceptive pill the last time they had sex. Fifteen per cent used the withdrawal method.
Four in ten (43 per cent) always used condoms when having sex over the previous year, 39 per cent did sometimes and 13 per cent never did. Of those who had access to a condom last time they had sex, 89 per cent of young men and 84 per cent of young women actually used it.
Those who didn’t use a condom most commonly said they were not prepared (27 per cent), trusted their partner (31 per cent), knew their partner’s sexual history (32 per cent) or didn’t like condoms (30 per cent).
Source: Parent Guides
Contraceptive implant
99.95% effective. The matchstick-sized implant sits under the skin of the arm and lasts up to three years. Inserted by a qualified health professional, it slowly releases a small amount of hormone.
Hormonal intrauterine device (IUD)
99.8% effective. This device is inserted into the uterus and lasts up to five years. It slowly releases very small amounts of hormone into the uterus.
Copper intrauterine device (Cu-IUD)
99.2% effective. This device is inserted into the uterus and lasts up to 10 years. It contains no hormones.
Vasectomy
99.85% effective (permanent). A vasectomy involves cutting the tubes that carry sperm, to stop sperm moving from the testes to the penis.
Female sterilisation
99.5% effective (permanent). Female sterilisation blocks the fallopian tubes, stopping eggs from moving down the tube and being fertilised. The most common methods are tubal ligation, (“having your tubes tied”), where a clip is put on each tube under general anaesthetic, and tubal occlusion, where a small coil (Essure) is put in each tube under local anaesthetic.

Source: GabiSandra / Pixabay
Combined pill
91% effective. The combined pill contains synthetic forms of the hormones oestrogen and progesterone. It stops ovulation and makes the fluid at the opening to the uterus thicker, stopping sperm from getting through.
Mini pill
91% effective. The mini pill contains a synthetic form of progesterone. It usually suits women who either have side effects when they take oestrogen or cannot take oestrogen for health reasons.
Vaginal ring
91% effective. The vaginal ring has similar hormones to the combined pill and works in the same way. A “one size fits all” ring is inserted into the vagina and stays there for three weeks, slowly releasing hormones that move from the vagina into the bloodstream.
Male condom
82% effective. One of the most accessible forms of contraceptive most commonly used by the general population.
Female condom
79% effective.
Diaphragm
This soft, shallow silicone dome fits in the vagina and covers the opening to the uterus, stopping sperm from getting through. It needs to stay in place for at least six hours after sex. If it is used, fitted and positioned correctly, a diaphragm is 94 per cent effective. They need to be fitted by a trained doctor or nurse and may not protect from STIs.
Emergency contraception
The morning-after pill is a hormonal method of contraception that may stop ovulation. It can be taken to avoid getting pregnant in an emergency situation, such as after having unprotected sex, if a condom slips off or breaks during sex or if the contraceptive pill is missed. It prevents 85 per cent of pregnancies. It is best to take emergency contraception as soon as possible, ideally within 24 hours of having sex.
Natural methods
Known as natural family planning, these methods monitor body changes during the menstrual cycle to identify when a woman is most fertile.
Injections
Depo-Provera and Depo-Ralovera are hormonal injections containing a progesterone-like hormone given every 12 to 14 weeks.
Abortion
In Victoria, abortion is legal up to 24 weeks without a doctor’s referral. After 24 weeks you can have an abortion if at least two doctors agree. The doctors must consider all relevant medical circumstances and your current and future physical, psychological and social circumstances.
Family Planning Victoria says you are not legally required to have counselling but can do so through your doctor, who can also refer you to a specially trained psychologist or nurse. FPV offers one-hour pregnancy choices information sessions with a nurse, which provide factual information about all the options available.
Edited text // Better Health Channel material is copyright © 2016. State of Victoria. Reproduced from the Better Health Channel (www.betterhealth.vic.gov.au) at no cost. The information published here was accurate at the time of publication and is not intended to take the place of medical advice. www.betterhealth.vic.gov.au/health/healthyliving/contraception-choices
Efficiency of contraception methods // Family Planning Alliance Australia. www.familyplanningallianceaustralia.org.au




